Explore the world of vectors, diseases, and the efforts made in Mauritius to mitigate their impact. It is a journey into the strategies, technologies, and community involvement that help protect Mauritians from vector-borne diseases and promote a healthier, more resilient nation. Join us in unraveling the story of vector-borne diseases and health in Mauritius, where science, action, and education converge to ensure a safer and more vibrant future.
Overview of Vector-Borne Diseases | ||
Vector-borne diseases are infectious diseases that are transmitted to humans or other animals through vectors such as mosquitoes, ticks, fleas, and sandflies. These vectors serve as intermediaries between infected individuals and new hosts. Common vector-borne diseases include malaria, dengue fever, Zika virus, and Lyme disease, among others. Critical Public Health ConcernThe link between environmental conditions and vector-borne diseases is a critical aspect of public health, particularly in regions like Mauritius. The nation faces unique environmental factors that influence the prevalence and spread of diseases carried by vectors such as mosquitoes and ticks. Mauritius' tropical climate, lush vegetation, and abundant water sources create ideal breeding grounds for disease-carrying vectors, making the understanding of these environmental conditions and their impact on vector-borne diseases a matter of paramount importance. Disease Management and PreventionThe link between environment and disease transmission is a complex interplay, shaped by factors ranging from climate and land use to human behavior. As a result, effective disease management and prevention strategies in Mauritius must consider the dynamic relationship between environmental conditions and vector-borne diseases to safeguard the health and well-being of its population. Like premature morbidity and mortality associated with traditional communicable, vector-borne diseases have significantly decreased in Mauritius. These achievements are attributed to the Integrated Surveillance System in place. However, challenges due to the resurgence of vector-borne diseases and emergence of new infectious diseases remain continuous threats to the country.
|  | |
Outbreaks of Vector-borne diseases in Mauritius | |||
The Ecological and Health Landscape of Mauritius - Interplay of Vector-Borne Diseases and Public HealthAmidst Mauritius's scenic beauty and vibrant communities, there lies a complex ecological balance that shapes the health and well-being of its residents. One crucial aspect of this equilibrium is the interplay between vector-borne diseases and public health. Vector-borne diseases are a significant concern in Mauritius, as they pose a substantial risk to the health of its people and the vitality of its ecosystems. These diseases, transmitted by vectors such as mosquitoes, ticks, and sandflies, can cause a range of illnesses, from malaria to dengue fever and more. Understanding the intricate relationship between vectors, diseases, and health is pivotal to safeguarding the nation's well-being. Mauritius's Battle Against Malaria - Malaria Elimination and Ongoing Vector ThreatsThe history of malaria in Mauritius is a testament to the island's resilience in facing vector-borne diseases and its ability to adapt to changing circumstances. From a time when malaria had a crippling impact on the population and economy, Mauritius has emerged as a model for successful malaria control and elimination, providing valuable lessons for the global fight against this deadly disease. In recent years, the island has witnessed sporadic outbreaks of other mosquito-borne diseases, such as dengue fever and chikungunya, underscoring the ongoing threat posed by Aedes mosquitoes. These outbreaks have necessitated renewed efforts in vector control, public health campaigns, and international collaboration to manage and prevent the spread of these diseases. Zika Virus Awareness and Prevention - Global Concern and Local VigilanceThere is no documented history of indigenous Zika virus transmission in Mauritius. However, it's important to note that Zika virus has been reported in several countries and regions across the world, particularly in tropical and subtropical areas where the Aedes mosquitoes, which are the primary vectors for Zika, are prevalent. Zika virus was first identified in the Zika Forest of Uganda in 1947. The virus remained relatively obscure for several decades, with sporadic cases reported in Africa and Southeast Asia. It was not until a significant outbreak in the Pacific Islands in 2007 that Zika virus gained more attention on the global stage. In 2015 and 2016, Zika virus garnered international concern due to its association with serious birth defects, particularly microcephaly, in babies born to infected mothers during pregnancy. The virus, primarily transmitted by Aedes mosquitoes, can also be transmitted through sexual contact and blood transfusion. Zika outbreaks occurred in various countries and territories in the Americas, including Brazil, which was significantly affected. These outbreaks led to heightened awareness and efforts to control the spread of the virus. While Mauritius has not reported indigenous Zika transmission, the island's government and health authorities likely remain vigilant about the potential introduction of the virus due to international travel and the presence of Aedes mosquitoes. Ongoing Challenges in Vector Control - Adapting to Dynamic ThreatsMauritius has a long history of proactive measures to control and manage vector-borne diseases, but the dynamic nature of these illnesses and their vectors requires continuous attention and adaptation. The preservation of public health in the face of vector-borne threats demands a holistic approach that integrates knowledge, prevention, and innovative solutions. Additionally, climate change and globalization can influence vector populations and disease transmission patterns, necessitating continuous monitoring, research, and adjustment of control measures.
| |||
Malaria | |||
Mauritius' Battle Against MalariaThe history of malaria in Mauritius is a testament to the island's long and arduous battle against this devastating vector-borne disease. Malaria, transmitted primarily by Anopheles mosquitoes, was once endemic in Mauritius and posed significant health challenges for the settlers, exposing the newcomers to the disease, resulting in significant morbidity and mortality. As Mauritius became a center for sugarcane cultivation and trade during the colonial period, the risk of malaria transmission increased due to environmental modifications, such as the creation of irrigation systems and wetlands for sugarcane cultivation. The disease had a profound impact on the labor force, impeding economic development and population growth. Strategies to Combat MalariaThe late 19th and early 20th centuries saw concerted efforts to combat malaria. Measures included draining mosquito breeding sites, larviciding, and quinine treatment for those infected. The environmental modifications aimed to reduce mosquito breeding habitats, and public health campaigns sought to raise awareness about the disease. Advances in medical science and healthcare, including the discovery of the parasite life cycle and the development of antimalarial drugs, particularly quinine and later synthetic drugs, were crucial in reducing the disease's impact. Malaria Elimination and Ongoing PreventionAs a result of these measures, Mauritius achieved a remarkable milestone - the elimination of indigenous malaria transmission by the mid-20th century. The last indigenous case was reported in 1997. Robust surveillance systems were established to detect and treat these cases promptly, preventing the reintroduction of malaria on the island. Today, the island continues to address the challenges posed by other vector-borne diseases, demonstrating a commitment to preserving public health and well-being. Continued Vigilance Against Imported CasesWhile local transmission was eliminated, Mauritius continued to face imported cases of malaria, primarily from travelers who had visited endemic regions. |
Anopheles
| ||
Symptoms (Malaria) | |||
Malaria is characterized by a range of symptoms, which can vary in severity depending on the specific Plasmodium species causing the infection and the individual's immune response. The typical symptoms of malaria include: Fever: Malaria often begins with a high fever, which is one of the hallmark symptoms of the disease. The fever can be cyclical, with recurring episodes of high temperature. Chills: Shivering and chills commonly accompany the fever and can be severe. Headache: Many individuals with malaria experience intense headaches. Muscle and Joint Pain: Similar to chikungunya, malaria can cause significant muscle and joint pain. Fatigue: Malaria often leads to extreme fatigue and weakness. Nausea and Vomiting: Nausea and vomiting are common symptoms, particularly during the onset of the disease. Sweating: Profuse sweating, especially during fever episodes, is a characteristic feature of malaria. Anemia: Malaria can lead to a decrease in red blood cells, resulting in anemia, which can cause fatigue, weakness, and pale skin. Enlarged Spleen and Liver: In some cases, the spleen and liver may become enlarged as a result of the infection. Cognitive Impairment: Severe malaria can affect cognitive function and may lead to confusion, seizures, or even coma. Malaria symptoms can be cyclic, with recurrent episodes of fever, chills, and sweating. The timing and intensity of these cycles depend on the species of the malaria parasite involved. For example, Plasmodium vivax and Plasmodium ovale infections can have 48-hour cycles, while Plasmodium falciparum and Plasmodium malariae infections may have 72-hour and 72- to 84-hour cycles, respectively. | |||
Chikungunya | |||
Overview of Chikungunya in MauritiusThe history of chikungunya in Mauritius is a relatively recent but significant chapter in the island's battle against vector-borne diseases. Chikungunya, caused by the chikungunya virus and primarily transmitted by Aedes mosquitoes, has had a notable impact on the health and well-being of the Mauritian population. Arrival and Spread of ChikungunyaChikungunya was not historically present in Mauritius, but the disease gained a foothold on the island due to international travel and the movement of infected individuals. The first recorded cases of chikungunya in Mauritius occurred in 2006, with the virus likely introduced by travelers returning from regions where the disease was prevalent. The disease quickly spread through the local mosquito population, Aedes albopictus, which are found on the island. These mosquitoes serve as vectors for the chikungunya virus, and their abundance in Mauritius contributed to the rapid transmission of the disease. Public Health Measures and ImpactResponse and Challenges Ongoing Prevention and PreparednessSurveillance and Control Lessons Learned and Future Strategies |
Aedes
Source: R. Boojhawon, H Runghen, R Nigel, SDDV Rughooputh, S Sungkur and M Ragavoodoo, 2006 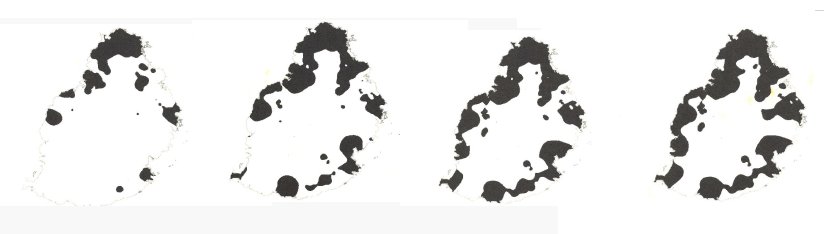 Propagation of the Chikungunya started from the coastal regions and progressed inland as shown in Figure. February was the most affected month and subsequently decreased. The latter may be a combination of weather conditions coupled with timely control measures introduced by the Ministries concerned to slow the progression. 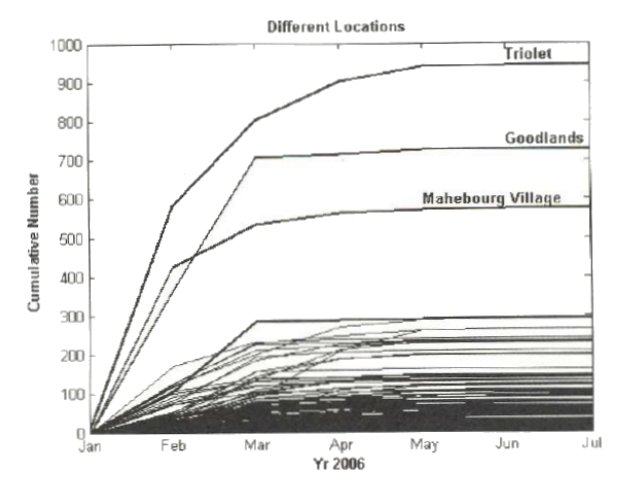 | ||
Symptoms (Chikungunya) | |||
The symptoms of chikungunya can be severe, and they often appear abruptly. While the disease is rarely fatal, the joint pain can be incapacitating, and the associated symptoms can have a significant impact on an individual's quality of life. Most people recover from chikungunya within a few weeks to months, but joint pain and arthritis-like symptoms can persist for an extended period in some cases. Chikungunya is characterized by a set of distinct symptoms, and the most common ones include: | |||
Sudden Onset of High Fever: Chikungunya typically begins with a sudden and high fever, often reaching temperatures of 102°F (38.9°C) or higher. Severe Joint Pain: The hallmark of chikungunya is intense joint pain, which can be debilitating and affect multiple joints. This symptom often gives rise to the disease's name, as "chikungunya" is derived from the Makonde language, meaning "to become contorted" or "bent up" in reference to the posture of patients with severe joint pain. Rash: Many individuals with chikungunya develop a rash, which can be itchy and typically presents as red, raised, and often maculopapular (small, flat, and raised) lesions. The rash may appear on the trunk, limbs, and sometimes the face. Headache: Chikungunya is commonly associated with severe headaches, which can be persistent and affect the quality of life.
| Muscle Pain: In addition to joint pain, individuals with chikungunya often experience muscle pain (myalgia), which can be generalized or localized to specific muscle groups. Fatigue: Chikungunya can lead to significant fatigue and weakness, making daily activities challenging. Swelling and Edema: Some people may experience swelling (edema) in the affected joints, leading to joint deformities and difficulties with mobility. Conjunctivitis: In some cases, chikungunya may cause conjunctivitis (inflammation of the eye's mucous membrane), leading to redness and eye discomfort. Nausea and Vomiting: Gastrointestinal symptoms, such as nausea and vomiting, can occur but are less common than the typical symptoms of fever and joint pain. Oral Ulcers: Some individuals may develop painful oral ulcers. | ||
Dengue | |||
Overview of Dengue in MauritiusThe history of dengue in Mauritius reflects the island's enduring battle against mosquito-borne diseases, particularly those transmitted by Aedes mosquitoes. Dengue, caused by the dengue virus, has had a notable impact on public health in Mauritius over the years. Dengue has a long history in Mauritius, with records of dengue-like outbreaks dating back to the early 19th century. At that time, the exact nature of the disease was not fully understood, and it was often referred to as "breakbone fever" due to the severe joint and muscle pain it caused. These early outbreaks had a significant impact on the island's population, as there were no vaccines or specific treatments available to combat the disease. Vector Dynamics and Public Health ResponseDengue remained sporadically present in Mauritius, and it was periodically responsible for outbreaks throughout the 20th century. The disease was associated with the presence of Aedes mosquitoes (Aedes albopictus) which served as vectors for the dengue virus. These mosquitoes found favorable breeding habitats on the island, and environmental changes, such as urbanization and changes in water storage practices, contributed to the proliferation of mosquito populations. Mauritius recognized the importance of addressing dengue and implemented various public health strategies to control the disease. These strategies included mosquito control programs, public education campaigns, and efforts to reduce mosquito breeding sites, such as stagnant water containers. The government worked to improve healthcare infrastructure and diagnostics to better manage dengue cases. Recent Trends and Ongoing EffortsResurgence and Continued Challenges Despite these efforts, Mauritius continued to experience dengue outbreaks. The disease presented challenges for the healthcare system, as severe cases required hospitalization, and in some instances, the healthcare system was strained by the number of dengue patients. Outbreaks occurred periodically, affecting residents and visitors to the island. In the early 21st century, Mauritius experienced a resurgence of dengue, with multiple outbreaks in the 2000s and 2010s. This resurgence prompted intensified control measures, including increased mosquito surveillance and vector control, as well as public health campaigns to raise awareness about dengue prevention. Check the latest statistics with regards to detected local cases and imported cases here. Persistence of Dengue and Prevention Focus Dengue remains a public health concern in Mauritius, as the island continues to face the risk of imported cases due to international travel and the presence of Aedes mosquitoes. The government and healthcare authorities have maintained ongoing efforts to manage and prevent the spread of the disease. The history of dengue in Mauritius underscores the persistent challenges posed by mosquito-borne diseases and the importance of comprehensive public health approaches to mitigate their impact. Mauritius has made significant progress in addressing dengue, but the risk of outbreaks persists, emphasizing the need for continued vigilance, international cooperation, and integrated strategies for mosquito control and disease prevention. |
Aedes
| ||
Symptoms (Dengue) | |||
Dengue is characterized by a set of distinct symptoms, which can vary in severity from mild to severe. The classic symptoms of dengue include: Sudden High Fever: Dengue often begins with a sudden and high fever, typically reaching temperatures of 104°F (40°C) or even higher. The fever is one of the hallmark features of the disease. Severe Headache: Intense headaches are a common symptom of dengue and can be extremely debilitating. Severe Joint and Muscle Pain: Dengue is often associated with severe joint and muscle pain, which has led to the term "breakbone fever." These pains can be very distressing. Rash: Many individuals with dengue develop a rash, which can vary in appearance but often presents as a maculopapular rash. This rash may appear a few days after the fever starts. Mild Bleeding: Some people with dengue experience mild bleeding, which can manifest as nosebleeds, gum bleeding, or easy bruising. In more severe cases, there may be internal bleeding, which requires immediate medical attention. Fatigue: Dengue can lead to significant fatigue and weakness. Nausea and Vomiting: Gastrointestinal symptoms, such as nausea and vomiting, are common. Swollen Lymph Nodes and Spleen: In some cases, individuals with dengue may develop swollen lymph nodes and an enlarged spleen. Conjunctivitis: Conjunctivitis, characterized by redness and discomfort in the eyes, can occur in some cases. | It's important to note that dengue can manifest in different forms, ranging from mild to severe. The severe form of dengue, known as dengue hemorrhagic fever (DHF) or dengue shock syndrome (DSS), can be life-threatening and is characterized by additional symptoms such as severe bleeding, circulatory system dysfunction, and organ failure. While most cases of dengue are mild and can be managed with supportive care, severe cases require immediate medical attention and hospitalization. Early diagnosis and appropriate medical care are critical for a positive outcome, particularly in severe cases. | ||
Vector-borne indicators
Disease Prevention through Environmental Management | |
Preventing vector-borne diseases through environmental management in Mauritius involves a multi-faceted approach aimed at reducing the breeding and proliferation of disease-carrying vectors, primarily mosquitoes, and ticks. The island's tropical climate, abundant water sources, and lush vegetation create ideal conditions for vector reproduction, making environmental management a critical component of public health. The strategies and measures employed for vector-borne disease prevention through environmental management in Mauritius include: | |
(A combination of these strategies, alongside international collaboration and a strong public health infrastructure, is essential to preventing vector-borne diseases through effective environmental management. This approach not only safeguards public health but also supports the island's tourism industry and overall quality of life for its residents.) Mosquito Control and Habitat Reduction:
Vegetation Control:
Water Quality and Water Storage:
Vector Surveillance and Monitoring:
Urban Planning and Infrastructure Design:
Public Health Awareness Campaigns and Education:
Integrated Vector Control Measures:
Research and Innovation:
International Cooperation:
|




